Types of Healthcare Services Patients Can Access in India
Outline
– Introduction: Why understanding India’s healthcare spectrum matters
– Section 1: Primary and community-based care
– Section 2: Secondary care and diagnostics
– Section 3: Tertiary and quaternary services
– Section 4: Complementary, rehabilitation, mental health, and palliative care
– Section 5: Access, affordability, and making informed choices
– Conclusion: Practical takeaways for patients and caregivers
Introduction
India’s health ecosystem blends public facilities, private providers, and a fast-growing digital layer. This mixed model gives patients many entry points, but it can also feel complex when illness strikes. Knowing which service suits which need—prevention, diagnosis, treatment, or recovery—can save time, money, and stress. The following guide walks through the major types of care, how they compare, and when each is most useful.
Primary and Community-Based Care: Your First Line of Support
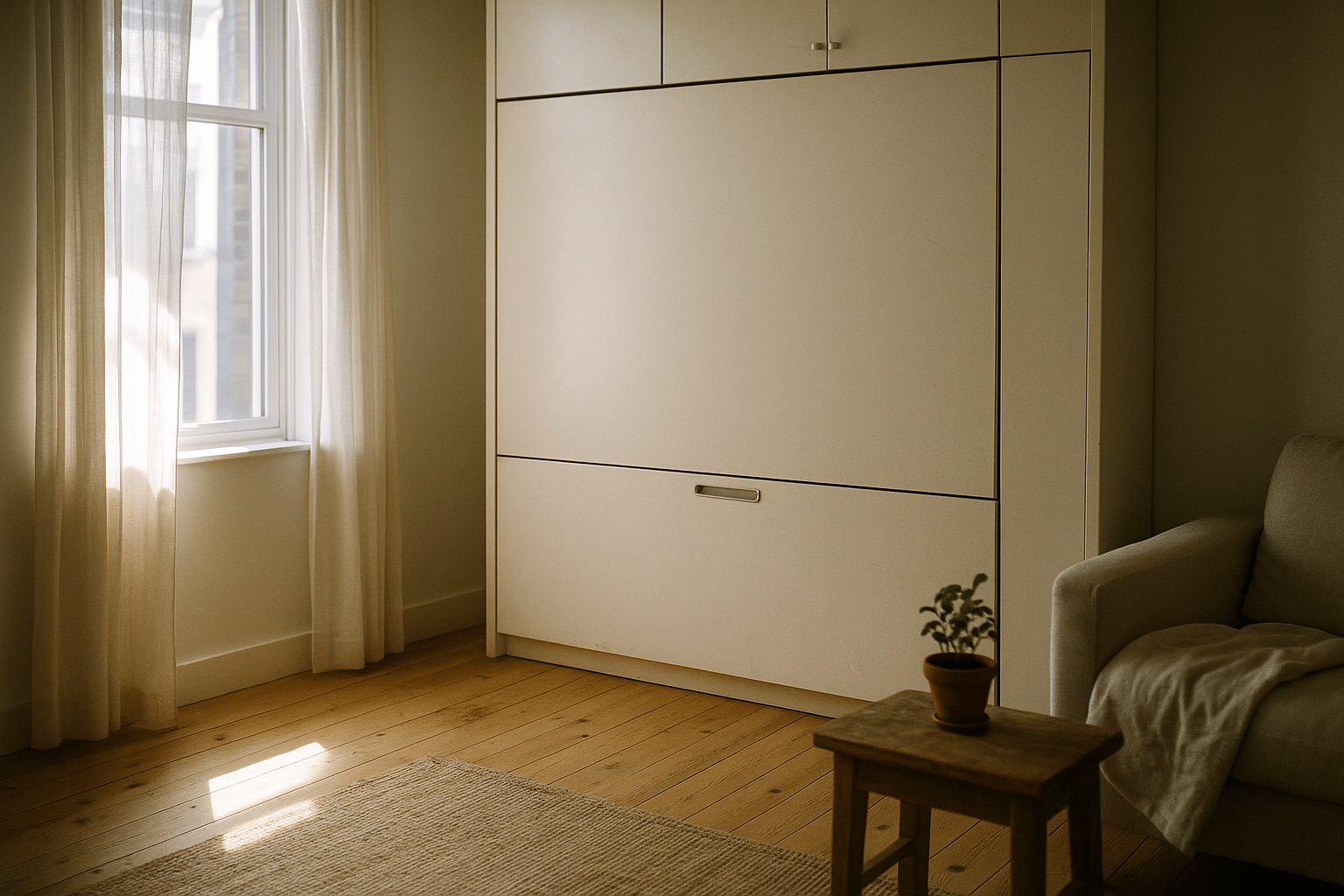
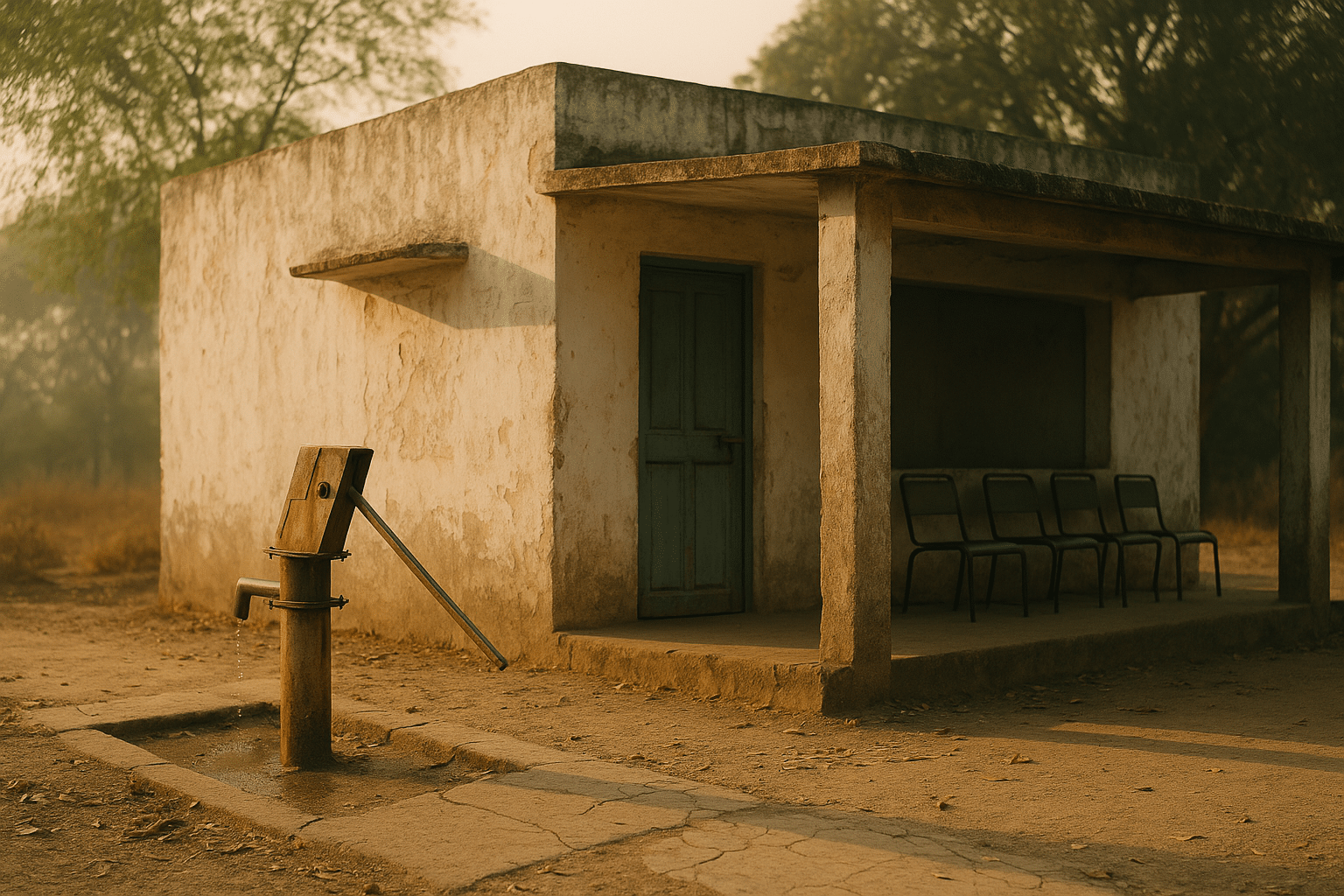
Primary care is the front door of India’s health system. It includes local clinics, solo and group practices, nursing stations, maternal and child health rooms, and public primary health centres in both rural and urban settings. These facilities focus on everyday needs: preventing illness, spotting problems early, and treating common conditions promptly. For many families, this is the most frequent and familiar touchpoint with the system—close to home, relatively affordable, and easier to visit without long waits.
What services are typical at this level? Many facilities offer the essentials:
– Preventive care such as immunisation, screening for blood pressure and diabetes, and health education.
– Basic outpatient consultations for coughs, fevers, skin infections, menstrual concerns, and minor injuries.
– Maternal and child health support, including antenatal check-ups, nutrition counselling, and growth monitoring.
– Essential medicines for common conditions and basic point-of-care tests (e.g., blood sugar, malaria rapid tests).
– Referral to higher-level centres when a case needs imaging, surgery, or specialist input.
Compared with higher tiers, primary care is designed for breadth rather than depth. It excels at continuity—seeing the same clinician over time—coordinating referrals, and following up on chronic conditions like hypertension or asthma. For patients, the advantages include shorter travel, lower costs, and a relationship-based approach that supports long-term health goals. The trade-off is that advanced diagnostics and specialised procedures are limited. When red flags appear—severe chest pain, complicated pregnancies, or neurological deficits—patients are guided up the referral ladder for faster testing and specialist care. People in India can access many different kinds of healthcare, from small neighbourhood clinics to large super speciality hospitals and digital teleco, and this first tier is the foundation that makes the rest work.
Secondary Care and Diagnostics: The Bridge Between Generalists and Specialists
Secondary care sits between primary clinics and high-complexity hospitals. District hospitals, multi-specialty nursing homes, and mid-sized private and public facilities typically offer a broader range of diagnostics and inpatient services. This is where imaging meets intervention: X-rays, ultrasound, CT scans, standard laboratories, and operating theatres for non-complex surgeries. Patients often arrive here via referral for conditions that need more than a general consultation but less than a tertiary centre’s intensive resources.
Key features you can expect at this level include:
– Specialist outpatient departments (e.g., general medicine, obstetrics and gynaecology, paediatrics, ENT, ophthalmology).
– Diagnostic suites for blood work, microbiology tests, and imaging beyond basic X-rays.
– Inpatient wards for moderate-risk cases and routine surgeries (e.g., appendectomy, hernia repair, uncomplicated fractures).
– Emergency rooms capable of stabilising trauma, heart-related symptoms, and acute infections before further referral.
– Rehabilitation starters such as post-operative physiotherapy planning.
How does secondary care compare with primary care? The scope is wider and infrastructure heavier: more beds, more equipment, and more specialists. Costs tend to be higher, and waiting times vary by location and demand. In many districts, secondary hospitals also serve as hubs for public health programmes, ensuring that vaccination campaigns and disease surveillance are coordinated with frontline clinics. Patients benefit from the mix of access and capability: you can get meaningful diagnostics and targeted treatment without always travelling to a metro. However, when a case becomes complex—intensive care needs, multi-organ issues, or rare diseases—the pathway leads to tertiary centres equipped for high-risk interventions.
Tertiary and Quaternary Care: Advanced Treatments and Super Specialities
Tertiary hospitals concentrate specialist expertise, high-end diagnostics, and advanced therapeutic options. These include super speciality departments such as cardiology, cardiothoracic surgery, neurosurgery, oncology, nephrology with dialysis and transplant services, and neonatal intensive care. Many functions are tightly integrated: comprehensive labs, interventional radiology, advanced imaging (MRI, PET-CT where available), and multi-disciplinary tumour boards or case conferences. Quaternary services push into ultra-specialised procedures and complex research-driven care pathways.
The strengths of tertiary care are depth and coordination. Multi-disciplinary teams can stage complex treatments—say, a cancer pathway that synchronises surgery, chemotherapy, and radiotherapy—with careful follow-up. Teaching and research arms often support updated protocols and clinical audits, which contribute to quality improvement. On the other hand, tertiary care can involve higher costs, longer travel, and the need for detailed documentation. It’s important to ask about clinical outcomes, infection control measures, and discharge planning—these indicators help families understand quality beyond glossy brochures.
When do patients need this level? Examples include major trauma requiring neurosurgery, advanced heart disease needing bypass or structural interventions, complicated pregnancies needing critical care, or rare disorders that demand sub-specialist input. Referral from primary or secondary providers is common and useful, because it packages prior labs and imaging into a coherent history. People in India can access many different kinds of healthcare, from small neighbourhood clinics to large super speciality hospitals and digital teleco, but this tier is where high-risk, high-benefit interventions are concentrated, and where getting a second opinion can be especially valuable.
Beyond Acute Care: AYUSH, Rehabilitation, Mental Health, Home-Based, and Palliative Services
Healthcare is more than hospitals. India’s landscape also includes systems of traditional and complementary care (collectively referred to as AYUSH), rehabilitation services, mental health care, home-based support, and palliative care. These offerings answer needs that stretch across prevention, function, and quality of life, especially for chronic or life-limiting conditions. Choosing among them requires attention to evidence, safety, and how each service fits into your overall care plan.
Complementary and traditional care is widely used for wellness, chronic pain, digestive issues, stress management, and musculoskeletal complaints. Patients should look for registered practitioners, discuss possible interactions with ongoing medicines, and set realistic goals. Rehabilitation services—physiotherapy, occupational therapy, and speech therapy—help people regain movement, independence, and communication after events such as stroke, injury, or surgery. Mental health offerings range from counselling and psychotherapy to psychiatric evaluation and medication management; privacy policies and continuity of care are essential considerations. Palliative care, whether inpatient or home-based, focuses on relief from pain and distress, shared decision-making, and caregiver support.
Helpful checkpoints when exploring these services:
– Verify credentials and registration status; ask about experience with your specific condition.
– Seek clarity on goals, timelines, and success indicators; good providers welcome these questions.
– Coordinate with your primary doctor to avoid conflicting treatments and to ensure medication safety.
– For home-based care, confirm emergency protocols, visit schedules, and equipment needs.
– For mental health and palliative care, ask about confidentiality, family meetings, and crisis plans.
Digital tools enhance access across this continuum. Teleconsultations can support follow-ups, therapy sessions, and caregiver coaching; remote monitoring can flag early changes in health status. Yet not all conditions are suitable for remote care—sudden weakness, severe pain, breathing difficulty, or confusion warrant in-person evaluation. Evidence-based practice remains the anchor: whether you choose physical therapy, mindfulness-based interventions, or pain management, align the plan with established guidelines and your personal goals.
Access, Affordability, and Smart Navigation: Choosing the Right Service at the Right Time
People in India can access many different kinds of healthcare, from small neighbourhood clinics to large super speciality hospitals and digital teleco, but smart navigation turns choice into real benefit. The core decisions revolve around urgency, complexity, and cost. For sudden, severe symptoms—chest pain, slurred speech, major injury—seek emergency services without delay. For non-urgent concerns, start with primary care; it is designed to triage, treat common conditions, and coordinate referrals. When tests or procedures exceed local capacity, step up to secondary or tertiary settings guided by your clinician.
Financing matters. Out-of-pocket spending still accounts for a significant share of total health expenditure in India, so it helps to map your options before a crisis. Consider:
– Public facilities, which may offer subsidised or free services based on eligibility and availability.
– Employer or group health coverage, which can reduce inpatient bills and offer cashless networks.
– Individual health insurance, which varies widely in premiums, exclusions, and pre-authorisation rules.
– Charitable trusts and social protection programmes that sometimes cover specific procedures or medications.
Practical steps to control costs and maintain quality:
– Ask for a written estimate; clarify what is included: surgeon fees, implants, ICU charges, and post-op medicines.
– Request an itemised bill and check for duplicate consumables.
– Inquire about alternatives: generic medicines, day-care procedures, or bundled packages.
– Seek a second opinion for major surgery or long-term therapies; it often refines the plan and may avoid unnecessary interventions.
– Keep copies of all reports; a portable medical record prevents repeat tests.
Quality and safety deserve equal attention. Look for infection control practices, emergency readiness, and patient feedback channels. Confirm how follow-up visits are scheduled and who to contact for complications. Digital options are useful for stable follow-ups, but physical examinations remain essential for new or worsening symptoms. Finally, align choices with your values: proximity versus comprehensiveness, cost versus speed, and continuity with a trusted clinician versus access to niche expertise.
Conclusion: Navigating Choices With Confidence
India’s healthcare spectrum is wide enough to meet most needs if you approach it with a plan. Start where the problem fits—primary for routine issues, secondary for broader diagnostics, and tertiary for complex care—while tapping supportive services that protect function and comfort. Budget ahead, keep your records, and ask clear questions about outcomes and costs. With informed decisions and timely referrals, families can turn a complex system into a pathway that works.